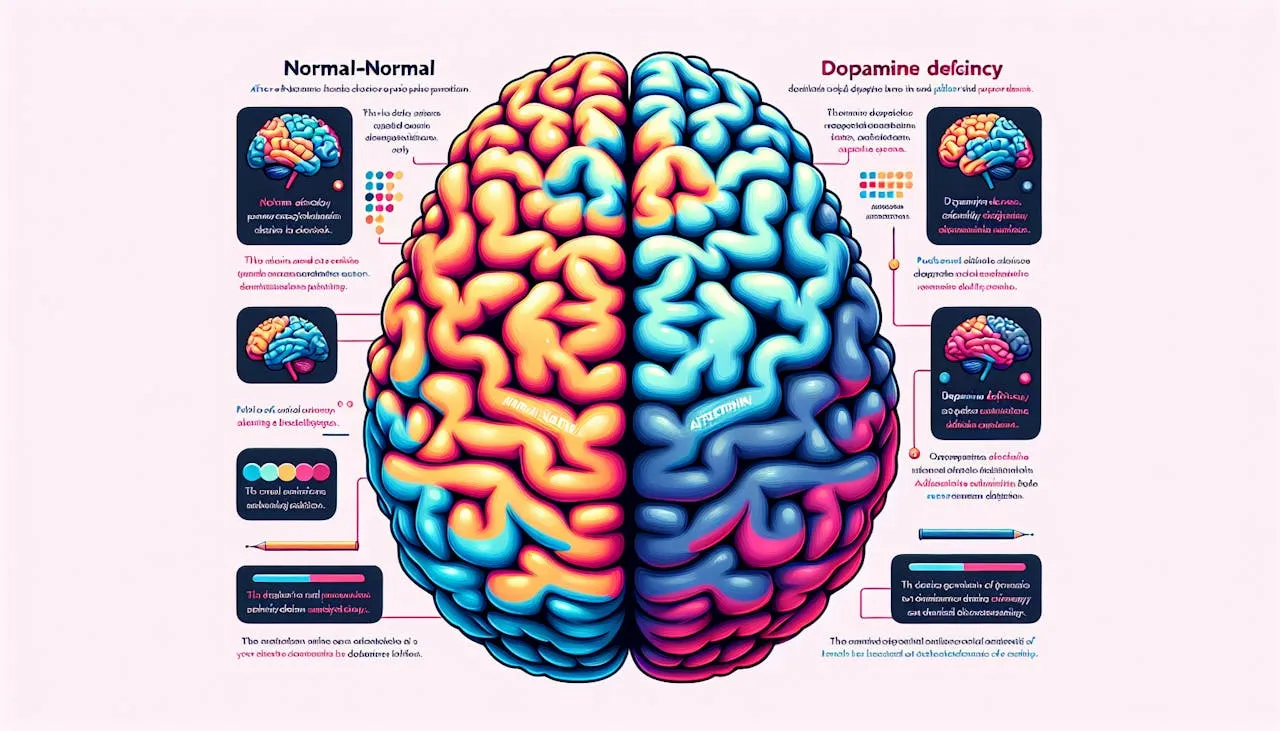
The Dopamine Deficiency Enigma
Unlocking the autism dopamine deficiency puzzle. Explore the link between dopamine and autism for a deeper understanding.
Understanding Autism Spectrum
Autism spectrum disorders (ASD) encompass a range of neurodevelopmental conditions that affect social interaction, communication, and behavior. Within the spectrum, individuals with autism often exhibit executive dysfunction, which includes difficulties with deliberate goal-directed behavior, planning, and cognitive flexibility in changing environments. This suggests that executive dysfunction is a central feature of autism.
Executive Dysfunction in Autism
Executive functions refer to a set of cognitive processes that enable individuals to plan, organize, and regulate their behavior to achieve specific goals. In the context of autism, executive dysfunction manifests as challenges in these processes. For instance, individuals with autism may struggle with shifting attention between tasks, adapting to new situations, and exhibiting inflexible behavior.
Research has shown that individuals with autism often face difficulties with cognitive flexibility, which refers to the ability to switch between different concepts or perspectives. One commonly used test to assess cognitive flexibility is the Wisconsin Card Sort Test (WCST). People with autism tend to perform poorly on this test, indicating their challenges in shifting cognitive strategies and adapting to changing rules.

Cognitive Flexibility Challenges
While individuals with autism may struggle with cognitive flexibility, some aspects of their executive function remain developmentally appropriate. For example, their fundamental cognitive control capabilities, such as inhibiting an inappropriate but relatively automatic response, show no significant impairment on many tasks.
Interestingly, individuals with autism exhibit a distinct pattern of executive dysfunction compared to other disorders. While they demonstrate reduced cognitive flexibility, their cognitive control abilities, such as those assessed by the Stroop task, appear relatively retained compared to healthy controls.
The XT model, a computational model of the prefrontal cortex, provides insights into this dichotomous pattern of behavior in autism. It suggests abnormalities in the dopamine-based modulation of frontal systems as a potential explanation. This model offers qualitative and quantitative fits to performance on cognitive control and cognitive flexibility tests in individuals with autism.
In summary, executive dysfunction, particularly cognitive flexibility challenges, is a prominent feature of autism spectrum disorders. Understanding the role of dopamine in modulating frontal systems can shed light on the underlying mechanisms contributing to these difficulties. Further research in this area may provide valuable insights into the development of targeted interventions for individuals with autism.
The Role of Dopamine in Autism
Dopamine, a neurotransmitter that plays a crucial role in various brain functions, has been implicated in the understanding of autism spectrum disorder (ASD). Research suggests that abnormalities in dopamine signaling and modulation contribute to the executive dysfunction observed in individuals with autism.
Prefrontal Cortex Abnormalities
Persons with autism often exhibit executive dysfunction, including challenges with deliberate goal-directed behavior, planning, and cognitive flexibility in changing environments. This suggests that executive dysfunction is a central feature of autism. The prefrontal cortex, a brain region responsible for higher-order cognitive functions such as decision-making and working memory, is particularly affected in individuals with autism.
Research using computational models, such as the XT model, suggests that abnormalities in the dopamine-based modulation of frontal systems may underlie the executive dysfunction seen in autism. This model explains the distinct pattern observed in autism, where individuals often struggle with cognitive flexibility but show relatively preserved cognitive control capabilities. Weakening the influence of dopamine on pyramidal cells in the prefrontal cortex can quantitatively capture the executive dysfunction seen in autism, supporting the role of dopamine in the prefrontal cortex abnormalities observed in individuals with ASD.
Dopamine-Based Modulation
Dopamine plays a critical role in modulating the functioning of the prefrontal cortex. It influences the communication between different neurons and brain regions, affecting cognitive processes such as attention, decision-making, and working memory. Research suggests that disturbances in dopamine-based modulation of frontal systems may underlie the executive dysfunction observed in autism.
While individuals with autism exhibit difficulties with tasks requiring cognitive flexibility, such as the Wisconsin Card Sort Test (WCST), they often show no significant impairment in fundamental cognitive control capabilities when compared to healthy controls. This unique pattern of reduced cognitive flexibility but relatively retained cognitive control differentiates the executive dysfunction observed in autism from other disorders.
Understanding the role of dopamine in autism is crucial for unraveling the complexities of the disorder and exploring potential avenues for intervention. Further research is needed to shed light on the specific dopaminergic anomalies and their impact on executive functioning in individuals with ASD.
Dopamine Hypothesis of ASD
The dopamine hypothesis of Autism Spectrum Disorder (ASD) suggests that abnormalities in dopaminergic function may contribute to the development and manifestation of autistic-like behaviors. Specifically, researchers have focused on the dysfunction of the midbrain dopaminergic system, particularly the medial striatum-prefrontal cortex (M-S-PFC) circuit [2].
Dopaminergic Anomalies in ASD
Studies have indicated that dopamine dysfunction is implicated in autism and may help explain certain symptoms observed in individuals with ASD, such as hyperactivity, tremors, and motor deficits. Variants in the dopamine transporter gene SLC6A3 have been identified in individuals with autism, affecting dopamine uptake and responsiveness to amphetamine. These variants can impact the function of the dopamine system, leading to altered neurotransmission.
Midbrain Dopaminergic System
The midbrain dopaminergic system plays a crucial role in regulating dopamine levels in the brain. Research has indicated that alterations in dopamine signaling within mesocorticolimbic and nigrostriatal circuits are associated with ASD. Specifically, there is evidence of reduced dopamine release in the prefrontal cortical area and diminished responsiveness of the nucleus accumbens in individuals with ASD.
Additionally, polymorphisms in dopamine receptor genes, particularly the D3 receptors, have been linked to repetitive and stereotyped behavior observed in individuals with ASD. These findings suggest that dopamine dysregulation may contribute to the core symptoms of ASD.
Understanding the dopamine anomalies and dysregulation in individuals with ASD is crucial for further research and potential development of targeted treatments. By exploring the role of dopamine in ASD, researchers aim to gain a deeper understanding of the neurobiological mechanisms underlying this complex disorder and pave the way for more effective therapeutic interventions.
Dopamine Dysregulation in Autism
Dopamine, a neurotransmitter known for its role in various brain functions, has been a subject of interest in understanding autism spectrum disorders (ASD). Research suggests that alterations in dopamine signaling may contribute to the core symptoms of ASD, including repetitive behaviors and impaired social interactions [4]. In this section, we will explore the dopamine-related dysregulations associated with autism, specifically focusing on dopamine signaling alterations and dopamine receptor polymorphism.
Dopamine Signaling Alterations
Recent studies have indicated that individuals with ASD exhibit altered dopamine signaling in specific brain circuits, such as the mesocorticolimbic and nigrostriatal pathways. These alterations manifest as reduced dopamine release in the prefrontal cortical area and diminished responsiveness of the nucleus accumbens in individuals with ASD. The prefrontal cortex plays a crucial role in executive functions, including cognitive flexibility and attention, which are often impaired in individuals with ASD. The dysregulation of dopamine signaling in these areas may contribute to the cognitive and behavioral symptoms observed in individuals with ASD.
Dopamine Receptor Polymorphism
Polymorphism in dopamine receptor genes has been linked to repetitive and stereotyped behaviors in individuals with ASD. Specifically, polymorphisms in dopamine D3 receptors have been associated with these symptoms. The D3 receptor subtype is primarily expressed in mesocorticolimbic circuits and plays a role in regulating motivation and reward-related behaviors. Altered function of these receptors may contribute to the repetitive and stereotyped behaviors observed in individuals with ASD.
Understanding the role of dopamine dysregulation and receptor polymorphism in ASD is crucial for developing targeted interventions and treatments. Pharmaceutical approaches that modulate dopamine signaling have shown promise in managing some of the symptoms associated with ASD. However, it is important to note that the application of these treatments should be based on careful evaluation and consideration of each individual's unique needs and circumstances.
Pharmacological Treatment for ASD
Antipsychotic Medications
Stimulant Medication Efficacy
In addition to investigating dopamine dysregulation in autism, researchers have explored pharmacological treatments to address the symptoms associated with ASD. Two commonly used classes of medications are antipsychotics and stimulants.
Antipsychotic medications, such as aripiprazole, have been approved by the FDA for the treatment of irritability in children and adolescents with ASD. Aripiprazole acts as a stabilizer of dopamine and serotonin within specific brain regions. Studies have shown its effectiveness in reducing irritability, hyperactivity, and stereotypies in individuals with ASD. However, it is important to consider potential side effects, such as weight gain and sedation, when using these medications.
Stimulant medications, commonly used to manage attention deficit hyperactivity disorder (ADHD), have also been explored for their efficacy in treating the symptoms of ASD. While stimulants can improve attention and hyperactivity in some individuals with ASD, their effectiveness in addressing core symptoms such as social communication deficits is limited. The response to stimulant medications can vary among individuals, and careful monitoring is necessary to assess their benefits and potential side effects.
It's important to note that medication should always be prescribed and monitored by a qualified healthcare professional. Each individual with ASD has unique characteristics and needs, so a personalized approach is crucial in determining the most appropriate pharmacological interventions.
Pharmacological Treatment for ASD
When it comes to managing the symptoms of Autism Spectrum Disorder (ASD), pharmacological interventions can play a crucial role. Two commonly used types of medications for ASD are antipsychotic medications and stimulant medications.
Antipsychotic Medications
Antipsychotic medications are often prescribed to address specific challenging behaviors associated with ASD, such as aggression, self-injuring behavior, temper tantrums, withdrawal, tics, and rituals in children with ASD. Second-generation antipsychotics (SGAs) are preferred over first-generation antipsychotics (FGAs) due to their lower risk of side effects.
Some commonly used antipsychotic medications for ASD include:
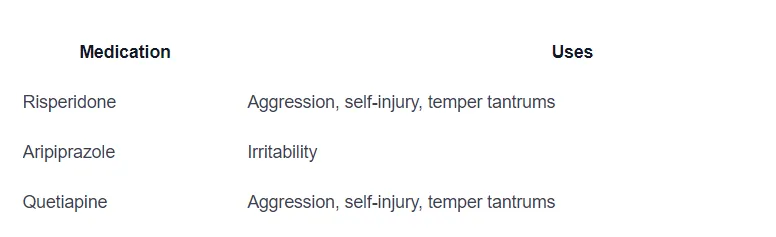
These medications work by modulating neurotransmitters, including dopamine and serotonin, in certain brain areas. It's important to note that while antipsychotic medications can be effective in managing challenging behaviors, they may also have potential side effects, such as weight gain, sedation, drooling, and tremor. Therefore, careful consideration and monitoring are necessary when using these medications.
Stimulant Medication Efficacy
Stimulant medications, such as methylphenidate, have shown efficacy in improving attention, cognitive functions, social communication, and self-regulation in children with ASD and comorbid ADHD. However, it's worth noting that the efficacy of stimulant medication in individuals with ASD may be lower compared to typically developing children with ADHD.
The dosage of stimulant medications for individuals with ASD should be carefully titrated, taking into consideration the specific needs and responses of each individual. The goal is to find the optimal dosage that maximizes the benefits while minimizing potential side effects. As with any medication, close monitoring and regular communication with healthcare professionals are essential.
Pharmacological treatment options for ASD, such as antipsychotic medications and stimulant medications, can be valuable tools in managing specific symptoms and improving the overall quality of life for individuals with ASD. However, it's crucial to consider a comprehensive treatment approach that includes behavioral interventions and individualized care to address the unique needs of each individual with ASD. Regular monitoring, ongoing assessment, and open communication between healthcare professionals, caregivers, and individuals with ASD are key to optimizing treatment outcomes.
Potential Dopamine Modulators
When it comes to addressing dopamine dysregulation in individuals with autism spectrum disorder (ASD), certain medications have shown promise as potential dopamine modulators. These medications aim to stabilize dopamine levels and improve symptoms associated with ASD. Two such medications are aripiprazole, brexpiprazole, and cariprazine.
Aripiprazole for ASD
Aripiprazole, an atypical antipsychotic medication, has been FDA-approved for the treatment of irritability in children and adolescents with ASD since 2009. It acts as a stabilizer of dopamine and serotonin within specific brain regions, including the nucleus accumbens, ventral tegmental area, and frontal cortex. Studies have shown that aripiprazole can be effective in reducing irritability, hyperactivity, and stereotypies in children and adolescents with ASD.
It is important to note that while aripiprazole can be beneficial, it is not without potential side effects. Weight gain and sedation are notable side effects that should be considered when prescribing this medication to individuals with ASD. Close monitoring and regular communication with a healthcare professional are essential to ensure the medication's effectiveness and manage any potential side effects.
Brexpiprazole and Cariprazine
Brexpiprazole and Cariprazine are two other medications that have shown potential as dopamine modulators in the context of ASD.
Brexpiprazole is a medication that acts as a partial agonist at D2/D3 receptors and as an antagonist at 5-HT2A and adrenergic alpha1B/2C receptors. While there are no specific studies exploring the efficacy of brexpiprazole in ASD, preclinical studies have shown its potential to improve social recognition deficits and facilitate social interactions, which are relevant to the core symptoms of ASD. Compared to aripiprazole, brexpiprazole has a lower tendency to cause side effects mediated by D2 partial agonism.
Cariprazine, another medication acting as a D2/D3 partial agonist, has shown dose-dependent efficacy in improving behavioral endpoints representing core and associated symptoms of ASD in animal models. Cariprazine has a high affinity for D3 receptors and acts as a D3-preferring D2/D3 partial agonist. Initial results suggest that cariprazine is well-tolerated and does not cause parkinsonism, although studies regarding its tolerability and safety in children and adolescents are limited. Cariprazine may hold promise as a medication for reducing intensive repetitive and stereotyped behaviors in ASD.
It is important to note that each individual with ASD is unique, and the effectiveness and tolerability of these medications may vary. The decision to prescribe any medication should be made in consultation with a healthcare professional who can assess the specific needs and circumstances of the individual. Regular monitoring and open communication are essential to ensure the benefits outweigh any potential risks.
By exploring potential dopamine modulators like aripiprazole, brexpiprazole, and cariprazine, researchers and healthcare professionals aim to develop targeted treatment approaches that address the dopamine dysregulation associated with ASD. Continued research in this area holds promise for better understanding and managing the symptoms of ASD.
References
- [1]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374973/
- [2]: https://www.sciencedirect.com/science/article/pii/S0074774223000867
- [3]: https://www.thetransmitter.org/spectrum/diverse-dopamine-defects-found-in-people-with-autism/
- [4]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8850940/
- [5]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8429404/
Does Your Child Have An Autism Diagnosis?
Learn More About How ABA Therapy Can Help
Find More Articles
Contact us
North Carolina, Nevada, Utah, Virginia
New Hampshire, Maine
Arizona, Colorado, Georgia, New Mexico, Oklahoma, Texas
.avif)