Unmasking the Most Common Psychiatric Disorders in Autism
Unmasking the most common psychiatric disorders in autism. Gain insights into the impact, prevalence, and treatment approaches.
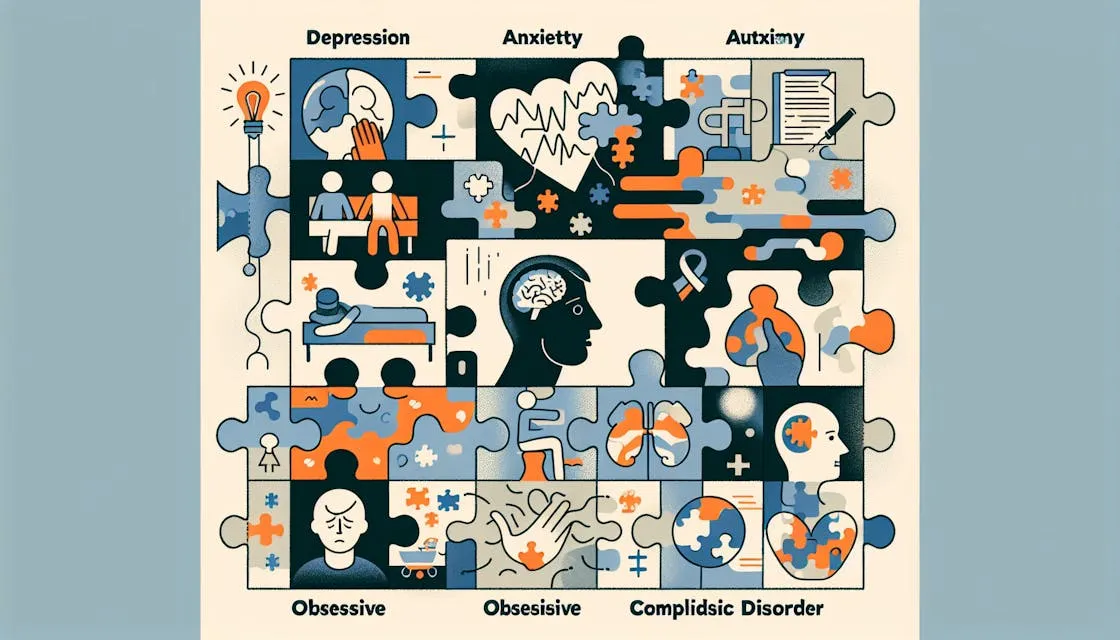
Common Psychiatric Disorders in Autism
Individuals with autism often experience comorbid psychiatric conditions, which refers to the presence of two or more disorders in the same individual. These psychiatric conditions can significantly impact the lives of autistic individuals and their families. Understanding the most common comorbid psychiatric disorders in autism is crucial for accurate diagnosis and effective treatment.
Overview of Comorbid Psychiatric Conditions
Research has shown that a significant number of individuals with autism also have comorbid psychiatric conditions. Some of the most common comorbid psychiatric disorders in autism include anxiety, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), and depression. These conditions often co-occur with autism and have a profound impact on the individual's overall well-being.

Challenges in Accurate Diagnosis
Accurately diagnosing comorbid psychiatric disorders in individuals with autism can be challenging. The varied presentations of emotion dysregulation in autism can complicate diagnostic decision making and may lead to inaccurate psychiatric diagnoses or delayed autism diagnosis, especially in high-functioning children.
One study found that approximately 60% of prior psychiatric diagnoses in children with high-functioning autism were not supported on the Autism Comorbidity Interview, suggesting potential misdiagnosis of psychiatric disorders in this population. This highlights the importance of specialized assessment tools and expertise in evaluating psychiatric disorders in individuals with autism.
To ensure accurate diagnosis, healthcare professionals need to consider the unique challenges and manifestations of psychiatric disorders in the context of autism. This may involve collaboration between professionals with expertise in both autism and psychiatry. Accurate diagnosis is crucial for developing tailored treatment plans that address the specific needs of individuals with comorbid psychiatric disorders and autism.
Understanding the common comorbid psychiatric conditions in autism and the challenges associated with their accurate diagnosis is essential for providing appropriate support and intervention for individuals with autism. By recognizing and addressing these comorbidities, healthcare professionals can help improve the overall well-being and quality of life for individuals on the autism spectrum.
Prevalence of Psychiatric Disorders
Psychiatric disorders commonly co-occur with autism spectrum disorder (ASD), impacting the well-being and quality of life of individuals with autism. Understanding the prevalence of these disorders is crucial for effective diagnosis and treatment. Let's explore the prevalence rates of some of the most common psychiatric disorders in individuals with autism: attention-deficit hyperactivity disorder (ADHD), anxiety, depression, bipolar disorder, and obsessive-compulsive disorder (OCD).
ADHD and Autism
Attention-deficit hyperactivity disorder (ADHD) is one of the most commonly reported co-occurring disorders in children and adolescents with ASD. Studies have shown that a significant proportion of individuals with ASD also meet the criteria for ADHD. In fact, in one study, 71% of children and adolescents with ASD met criteria for any ADHD presentation.
Anxiety and Depression
Anxiety and depression are prevalent psychiatric disorders among individuals with autism. Research has shown that individuals with autism have a higher prevalence of anxiety (22.40%) and depression (25.90%) compared to the general population. These conditions can significantly impact the daily functioning and overall well-being of individuals with autism.
Bipolar Disorder and OCD
Bipolar Disorder and Obsessive-compulsive disorder (OCD) are also observed at higher rates among individuals with autism compared to the general population. In a study, the prevalence of bipolar disorder among autistic adults was found to be 2.50%. The prevalence of OCD among autistic adults was found to be 3.02%.
It is important to note that these psychiatric conditions occur at significantly higher rates in autistic individuals compared to the general population. Co-occurring psychiatric disorders can present challenges in accurate diagnosis and appropriate treatment, as symptoms can overlap and interact with each other.
By understanding the prevalence of these psychiatric disorders in individuals with autism, healthcare professionals can better tailor interventions and treatments to address the specific needs of each individual. Early identification and appropriate management of these co-occurring disorders are essential for promoting the well-being and overall mental health of individuals with autism.
Impact of Misdiagnosis
When it comes to individuals with autism, accurate diagnosis of psychiatric disorders is crucial for providing appropriate support and treatment. However, misdiagnosis can occur, leading to various negative consequences. In this section, we will explore two significant impacts of misdiagnosis: inappropriate treatments and higher medication usage.
Inappropriate Treatments
Research has shown that approximately 60% of prior psychiatric diagnoses in children with high-functioning autism were not supported by the Autism Comorbidity Interview, suggesting a high rate of misdiagnosis. Varied presentations of emotion dysregulation in autism can complicate diagnostic decision making, potentially leading to inaccurate psychiatric diagnoses or delayed autism diagnosis for high-functioning children.
When a child with autism is misdiagnosed with a psychiatric disorder, they may receive treatments that are not specifically tailored to their needs. Inappropriate treatments can result in ineffective or even detrimental outcomes. Misdiagnosis may lead to valuable time and resources being directed towards interventions that may not address the core challenges associated with autism.
Higher Medication Usage
Inaccurate psychiatric diagnoses in children with autism can also contribute to higher medication usage. Studies have found that the majority of children with autism spectrum disorders (ASD) meet criteria for at least one concurrent psychiatric disorder, with comorbidity rates being even higher in samples of referred youth. However, there is a high rate of false positive diagnoses of comorbid disorders in children with ASD, leading to inappropriate treatments and delayed diagnosis of ASD.
Misdiagnosis may result in the prescription of medications that are intended to target the misdiagnosed psychiatric disorder but may not be suitable or necessary for the individual's actual needs. This can lead to potential side effects, increased medication burden, and unnecessary exposure to medications that may not provide the desired benefits. In some cases, misdiagnosis can even lead to a higher likelihood of psychiatric hospitalization.
It is important to emphasize the significance of accurate diagnosis in individuals with autism and comorbid psychiatric disorders. Proper assessment and evaluation by professionals who specialize in both autism and psychiatry can help minimize the risk of misdiagnosis, ensuring that individuals receive the most appropriate and effective treatments for their specific needs.
Neurological Conditions in Autism
While autism is primarily characterized by challenges in social communication and repetitive behaviors, individuals with autism often experience comorbid psychiatric and neurological conditions. In this section, we will explore two neurological conditions that are commonly seen in individuals with autism: epilepsy and psychosis/schizophrenia.
Epilepsy and Autism
Epilepsy, a neurological disorder characterized by recurrent seizures, is significantly more common in autistic individuals compared to the general population. According to a study published in the NCBI, epilepsy is approximately 9.21 times more prevalent in individuals with autism. The co-occurrence of epilepsy and autism can present unique challenges in diagnosis and treatment.
Seizures in individuals with autism can manifest in various forms, such as generalized tonic-clonic seizures, absence seizures, or focal seizures. It is essential for healthcare professionals to be aware of this association and consider the possibility of epilepsy when evaluating individuals with autism.
Psychosis and Schizophrenia
There is a high comorbidity between autism and psychosis, including symptoms associated with schizophrenia. Research suggests that up to 34.8% of individuals with Autism Spectrum Disorder (ASD) exhibit psychotic symptoms. It is important to note that these symptoms may differ from those typically seen in individuals without autism.
When identifying comorbid psychosis in individuals with ASD, key dimensions to consider are delusions, hallucinations, and negative symptoms. However, it is crucial to differentiate between genuine psychosis and sensory anomalies or anomalous perceptual experiences commonly reported in individuals with ASD. Misinterpretation of these sensory experiences as hallucinations can lead to inaccurate diagnoses.
Understanding and addressing the comorbidity between autism and neurological conditions such as epilepsy and psychosis is essential for providing comprehensive care to individuals on the spectrum. Collaborative efforts between healthcare professionals from different specialties can help tailor interventions for the unique needs of individuals with autism and these comorbid conditions.
As research in the field of autism continues to evolve, there is a growing recognition of the need for evidence-based interventions to support mental health in autistic individuals, particularly adults. By advancing our understanding of the relationship between autism and neurological conditions, we can work towards developing more effective interventions and improving the quality of life for individuals on the autism spectrum.
Treatment Approaches
When it comes to addressing the psychiatric disorders that often coexist with autism, there are various treatment approaches available. Psychotherapy, including cognitive behavioral therapy (CBT) and mindfulness-based interventions, has shown promise in helping autistic individuals manage their mental health challenges.
Psychotherapy for Autistic Individuals
Psychotherapy is a valuable tool in helping autistic individuals navigate and cope with troubling thoughts, feelings, and behaviors. It provides a supportive environment where individuals can work with a trained therapist to explore their emotions, develop coping strategies, and enhance their overall well-being. Research indicates the benefits of psychotherapy for autistic individuals, although further studies are needed to test the effectiveness of specific treatments, especially among those with more significant intellectual and communication differences.
Cognitive Behavioral Therapy (CBT) and Mindfulness-Based Interventions
Cognitive behavioral therapy (CBT) is a widely recognized form of psychotherapy that focuses on the connection between thoughts, feelings, and behaviors. It has been proven effective in reducing anxiety and depression among individuals on the autism spectrum. Modified versions of CBT have shown promise in improving the mental well-being of autistic individuals with minimal to no intellectual or communication challenges. By addressing negative thought patterns and developing healthier coping mechanisms, CBT helps individuals manage their symptoms and improve their quality of life.
Mindfulness-based interventions, such as Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), have also demonstrated potential in reducing distress and enhancing well-being in non-autistic individuals. Although research in this area is still limited, these interventions appear promising in alleviating distress among autistic adults with minimal to no intellectual or communication challenges. By promoting self-awareness and acceptance, mindfulness-based interventions can help individuals develop effective strategies for managing their mental health.
While not specifically mentioned in the extra context, it is worth noting that interpersonal psychotherapy (IPT), a well-established approach for treating depression in non-autistic individuals, has shown effectiveness in treating depression in young people with autism. IPT focuses on the relationship between an individual's mood and their social interactions. However, further research is needed to understand the application of IPT in areas beyond negative mood or feelings, especially in relation to other challenges that autistic individuals may face.
By utilizing psychotherapy approaches like CBT, mindfulness-based interventions, and potentially IPT, autistic individuals can gain valuable tools to manage their mental health challenges. It's important to remember that each person is unique, and treatment approaches should be tailored to the individual's specific needs and strengths. Working with qualified professionals can help ensure that the chosen treatment approach aligns with the individual's goals and helps them lead fulfilling lives.
Future Research and Considerations
As we continue to gain a deeper understanding of psychiatric disorders in individuals with autism, it is crucial to prioritize future research and consider the development of evidence-based interventions. The following areas warrant attention and exploration:
Need for Evidence-Based Interventions
Currently, there is a lack of evidence-based interventions specifically tailored to supporting mental health in autistic adults. In a review of interventions, none were rated as 'evidence-based,' and some were 'not recommended'. This highlights the importance of conducting rigorous research to identify effective treatment approaches. Evidence-based interventions can provide a solid foundation for healthcare providers and individuals with autism to make informed decisions about suitable treatments.
To address this gap, future research should focus on developing and evaluating interventions that are tailored to the unique needs and priorities of autistic individuals. It is essential to consider the acceptability of interventions to the autistic community and involve autistic individuals in the research process. By embracing a collaborative approach, we can ensure that interventions are effective, relevant, and positively impact the mental health of autistic individuals.
Tailoring Treatments for Autistic Individuals
In the realm of psychotherapy, there is growing recognition that adjustments need to be made to accommodate the specific characteristics and needs of autistic individuals. Tailoring treatments for autistic individuals involves various considerations, including:
- Focusing on positive character attributes and strengths of the individual.
- Accommodating autism-related traits on an individual basis.
- Clarifying the individual's preferred terms related to autism and mental health.
- Incorporating special interests to teach and engage.
- Using written and visual information, along with structured worksheets.
Additionally, providing psychoeducation about the relationship between autism and mental health, exploring and developing emotional awareness/recognition, emphasizing behavioral strategies, and supporting healthy lifestyle behaviors are important components of psychotherapeutic approaches for treating co-occurring mental health conditions in autistic individuals.
Specific psychotherapeutic approaches that have shown promise for autistic individuals include:
- Cognitive Behavioral Therapy (CBT): A well-established approach that focuses on the role of thoughts and behaviors in influencing emotions. Modified versions of CBT have been effective for autistic individuals with minimal to no intellectual or communication challenges.
- Mindfulness-Based Interventions: These interventions, such as Mindfulness Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), have shown promise in reducing distress and facilitating well-being among autistic adults. However, more research is needed to assess their effectiveness for autistic individuals.
- Interpersonal Psychotherapy (IPT): A well-established approach for treating depression in non-autistic adults and youth. Further research is needed to understand its application in relation to other areas causing challenges in autistic individuals.
By tailoring treatment approaches to the specific needs and characteristics of autistic individuals, we can optimize the effectiveness of interventions and promote better mental health outcomes. Continued research and refinement of treatment strategies will ultimately contribute to improved well-being for individuals with autism and co-occurring psychiatric disorders.
References
- https://meta.stackexchange.com/questions/189920/what-is-the-3-x-backquote-markdown-used-for
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601822/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6669096/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10482712/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8918655/#__sec24title
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8918655/#__sec32title
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8918655/#__sec40title
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0273534
- https://aidecanada.ca/resources/learn/mental-health/treating-mental-health-conditions-in-autistic-individuals-a-toolkit-for-understanding-approaches-to-mental-health-care/
Does Your Child Have An Autism Diagnosis?
Learn More About How ABA Therapy Can Help
Find More Articles
Contact us
North Carolina, Nevada, Utah, Virginia
New Hampshire, Maine
Arizona, Colorado, Georgia, New Mexico, Oklahoma, Texas
.avif)